Coagulation and Fibrinolysis
The function of platelets
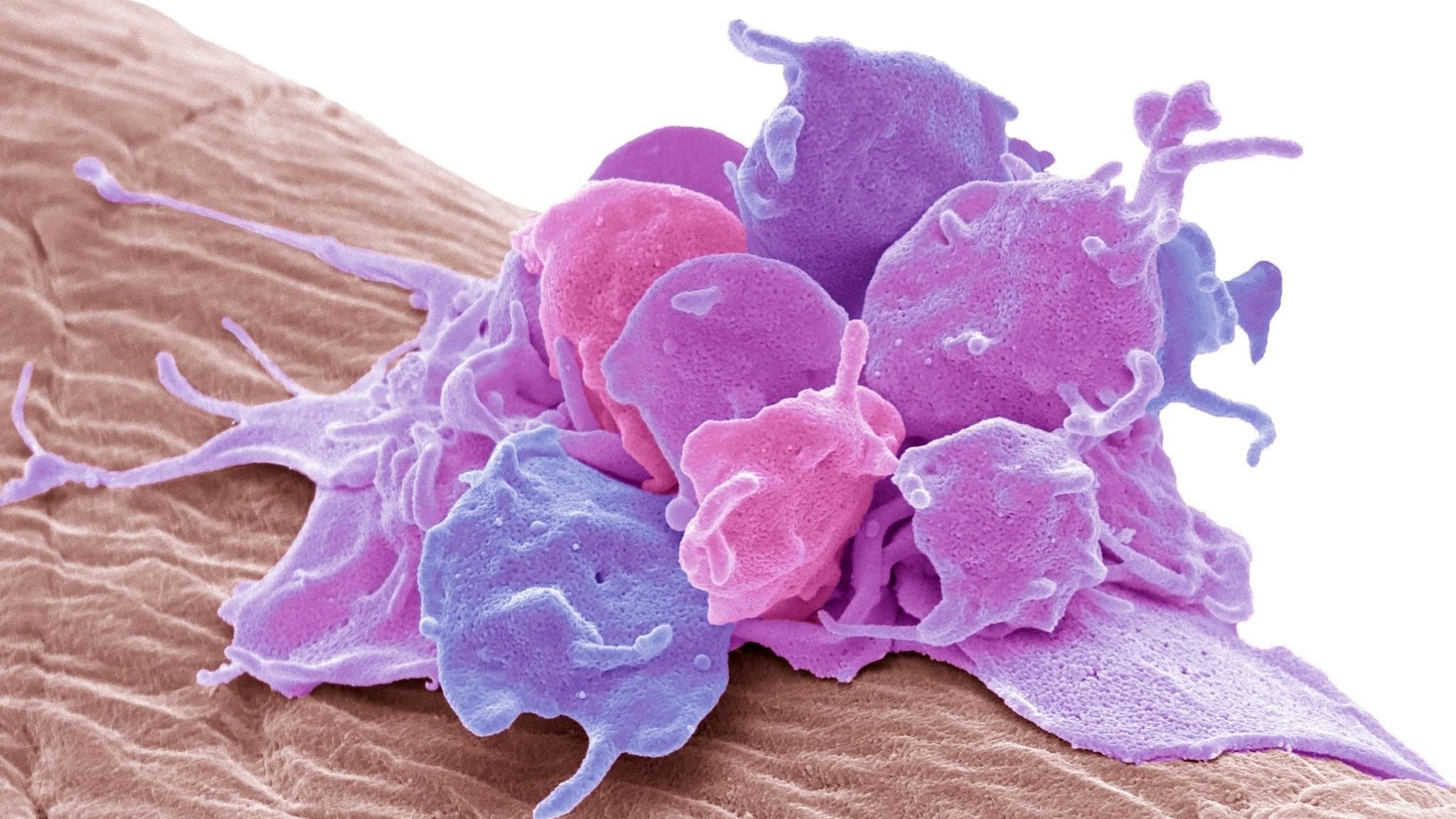
Platelets play an important role in blood coagulation and hemostasis. Hemostasis is the body's natural response to a bleed-inducing injury. Platelets are little non-nucleated cells. They are synthesized in the bone marrow from megakaryocytes and circulate throughout the vascular system, where they play an important role in hemostasis and thrombosis. After red blood cells, platelets are the second most prevalent cells in a healthy person (Seyoum et al., 2018). If there is damage to vascular tissue, then the subendothelial collagen is revealed. Platelets and endothelial cells produce large plasma protein von Willebrand factor (vWF), which binds to the collagen and forms the bridge between platelets and the collagen. This action leads to platelet activation. Platelets that have been stimulated produce a range of substances, expand and develop spiked processes, and become stickier (Marieb et al., 2018, p.658). Von Willebrand factor is a large glycoprotein present in the plasma and endothelium that binds to other proteins, particularly factor VIII, preventing them from rapidly decomposing. Also, platelets may release chemical messengers such as adenosine diphosphate (ADP), which acts as an aggregating agent which causes more platelets to stick to the injury area and release their chemicals (Seyoum et al., 2018). Furthermore, there are other two regulatory mediators, serotonin and thromboxane. These messengers increase vascular spasm and platelet aggregation, which reduces bleeding and aids in blood clotting.
The process of fibrinolysis
Fibrin is both the first product of the coagulation cascade and the ultimate substrate for fibrinolysis; hence it is critical for hemostasis. Clot shape, fibrinogen isoforms and polymorphisms, the rate of thrombin synthesis, and the general biochemical environment all have a role in fibrinolysis effectiveness. A diverse set of cofactors, receptors, and inhibitors regulate fibrinolysis. Fibrinolytic activity can be produced on the surface of a fibrin-containing thrombus or on cells with profibrinolytic receptors. Acquired and congenital abnormalities in fibrinolysis contribute to disease morbidity in a growing number of clinical illnesses (Chapin et al., 2015). Enzyme plasmin is the major clot destructor, and it is activated from plasminogen, the inactive form of plasmin, which is produced in the liver, then circulates in the blood. Plasminogen activator factors are produced by endothelial tissue when are stimulated by cytokines and hormones. The process of fibrinolysis starts about two days after the injury and lasts several days until the clot has dissolved (Marieb et al., 2018, p.660).
Chapin, J. C., & Hajjar, K. A. (2015). Fibrinolysis and the control of blood coagulation. Blood reviews, 29(1), 17–24. https://doi.org/10.1016/j.blre.2014.09.003
Marieb, E. N. (2018). The function of blood and its constituents. In Human Anatomy and Physiology (pp. 643-730). Pearson.
Seyoum, Enawgaw, B., & Melku, M. (2018). Human blood platelets and viruses: defense mechanism and role in the removal of viral pathogens. Thrombosis Journal, 16(1), 16–16. https://doi.org/10.1186/s12959-018-0170-8
Zampieri, Ranzani, O. T., Sabatoski, V., de Souza, H. P., Barbeiro, H., da Neto, L. M. C., Park, M., & da Silva, F. P. (2014). An increase in mean platelet volume after admission is associated with higher mortality in critically ill patients. Annals of Intensive Care, 4(1), 1–8. https://doi.org/10.1186/s13613-014-0020-1